Emergency Department
Anaesthesia Techniques for Manipulation
Introduction
Different anaesthesia techniques have been used to reduce DRFs in the Emergency Department. Local factors, such as the capability of the on-duty personnel in the Emergency Department and availability of resources to undertake any particular technique, dictates to a large extent which of the methods is commonly employed in each individual department. The aim is to review the anaesthetic techniques used to reduce the fracture and/or stabilise it.
Review Question
How does manipulation performed under general anaesthesia compared to wide awake manipulation (using either a haematoma block or IVRA) affect quality of reduction / functional outcome?
|
Population
|
Adults ≥16yrs of age or older requiring manipulation in the emergency department for a fracture of the distal radius
|
|
Intervention
|
Manipulation under Regional Anaesthesia
|
|
Comparison
|
Manipulation under General Anaesthesia
|
|
Outcomes
|
PROMs
Functional outcome
Complications
|
|
Study Designs
|
Meta-analyses, systematic reviews, RCTs, cohort studies
|
Evidence
There is a Cochrane review of the various methods of anaesthesia used for treating distal radius fractures. It includes the only randomised controlled trial comparing general anaesthesia with haematoma block with or without sedation.
Due to the paucity of RCTs comparing general with regional anaesthesia, evidence was also sought from studies comparing different techniques of wide awake anaesthesia. The available studies have been reviewed under the following categories:
A) General Anaesthesia versus haematoma block one trial. View here
B) Intravenous regional anaesthesia (IVRA) versus haematoma block- five trials. View here
Evidence Statement
Level 1:
Primary question (GA vs haematoma block)- Extremely limited evidence which suggests that there is no difference in the quality of reduction for GA versus haematoma block with patients in the latter group reporting more pain during manipulation, whereas patients undergoing manipulation under GA experienced more post- manipulation pain.
Level 1:
Secondary question (IVRA vs haematoma block)- IVRA is associated with better correction of the deformity with less pain when compared to manipulation under haematoma block.
Recommendation
Grade of Recommendation: Grade C
Best Practice Point:
The GDG supports the NICE guidelines to consider intravenous regional anaesthesia (Bier's block) when reducing dorsally displaced DRFs in adults (16 or over) in the emergency department. As there are known complications of IVRA, this should be performed by healthcare professionals trained in the technique, who need not necessarily be anaesthetists. (NICE non-complex fracture guidelines: https://www.nice.org.uk/guidance/NG38/chapter/Recommendations#ongoing-orthopaedic-management
If suitably qualified and trained personnel are not available to perform IVRA, haematoma block is a safe and reasonable option to reduce the fracture. However, given that IVRA, through superior pain relief, allows the manipulator to achieve a better quality of fracture reduction, patients should be offered the opportunity to wait up to 72 hours for the availability of suitably qualified personnel. The use of gas and air (nitrous oxide and oxygen) on its own provides inadequate pain relief and is not recommended.
Does manipulation affect functional outcome?
Introduction
Displaced DRFS are frequently manipulated in the emergency department to improve the position of the fracture. The aim is to review whether manipulation of a fracture of the distal radius compared to no manipulation affects patient reported or functional outcome scores.
Review Question
How does intervention with manipulation compared with no manipulation affect the patient reported outcome/functional outcome of the patient?
|
Population
|
Adults ≥16yrs of age who have sustained a displaced fracture of the distal radius
|
|
Intervention
|
Manipulation
|
|
Comparison
|
No manipulation
|
|
Outcomes
|
PROMs
Functional outcome
Complications
|
|
Study Designs
|
Meta-analyses, systematic reviews, RCTs, cohort studies
|
Evidence
A total of five papers were reviewed for this question, including one systematic review, 1 RCT and three case series. Two met our inclusion criteria. View here.
Evidence Statement
Level 1
For fractures of the distal radius in patients aged ≥50 years with moderately displaced fractures there is evidence for those over the age of 65 years that manipulation may not improve functional outcome, stiffness, final radiological position or cosmesis compared to no manipulation.
There is no evidence available for patients under 65 years.
Recommendation
Grade of Recommendation: Grade C
Manipulation may not improve outcome in patients aged 65 years or older with moderately
displaced fractures.
Full cast versus back slab immobilisation
Introduction
The aim is to review how a full cast compares to a back slab in maintaining reduction and in terms of maintenance of reduction and patient reported or functional outcome scores.
Review Question
How does a full cast compared to a back slab affect the maintenance of the reduction and patient reported outcome / functional outcome?
|
Population
|
Adults ≥16yrs of age who have sustained a dorsally displaced fracture of the distal radius
|
|
Intervention
|
Immobilisation in a full cast after closed reduction
|
|
Comparison
|
Immobilisation in a back slab after closed reduction reduction
|
|
Outcomes
|
Maintenance of reduction
PROMs
Functional outcome
Complications
|
|
Study Designs
|
Meta-analyses, systematic reviews, RCTs, cohort studies
|
Evidence
There is only one randomised controlled trial that fulfils the exact criteria set out in the question i.e. immobilisation in a full cast is compared to a back slab.
Evidence Statement
Level 3:
The number of patients in the only RCT available for review is not sufficient to draw meaningful conclusions.
Recommendation
Best Practice Point:
Immobilisation can be adequately achieved either by the use of a full cast or by use of a back slab depending on the expertise of the personnel carrying out the application of the splint and the preference of the patient. The GDG recommends that the patient is provided with a written care sheet with emergency contact numbers as per BOAST guidelines for DRFs.
Vitamin C for prevention fo complex regional pain syndrome (CRPS)
Introduction
CRPS is a complication which may be seen after a distal radius fracture characterised by severe pain, swelling and skin changes. Vitamin C has been advocated as a cheap, safe and effective treatment to prevent CRPS following injury or surgery. The aim is to review whether treatment with Vitamin C compared with placebo prevents CRPS in patients with a fracture of the distal radius.
Review Question
How does Vitamin C compared to placebo affect rates of CRPS?
|
Population
|
Adults ≥16yrs of age who have sustained a fracture of the distal radius
|
|
Intervention
|
Oral Vitamin C therapy
|
|
Comparison
|
Placebo
|
|
Outcomes
|
CRPS
PROMs
Functional outcome
Complications
|
|
Study Designs
|
Meta-analyses, systematic reviews, RCTs, cohort studies
|
Evidence
A total of 38 papers were reviewed for this question, including three meta analyses and three RCTs. Six papers met the inclusion criteria. View here.
Evidence Statement
Level 1++:
For adult patients with a distal radius fracture, there is no evidence that treatment with Vitamin C prevents CRPS when compared to placebo.
Recommendation
Grade of Recommendation: Grade A
Vitamin C is not recommended for the prevention of CRPS in patients with DRFs.
Radiological Parameters and Outcome
Introduction
Several parameters are commonly measured on radiographs of DRFs. The aim is to review whether any of these parameters seen on radiographs influence the patient reported or functional outcome of the patient.
Review Question
Which radiological parameters affect the patient reported outcome/functional outcome of the patient?
|
Population
|
Adults ≥16yrs of age or older with a fracture of the distal radius
|
|
Intervention
|
not applicable
|
|
Comparison
|
Radiological parameters; dorsal tilt, radial inclination, radial length, ulnar variance, intra-articular step and gap
|
|
Outcomes
|
PROMs
Functional outcome
|
|
Study Designs
|
Meta-analyses, systematic reviews, RCTs, cohort studies, case series
|
Evidence
No randomised controlled trials or cohort studies were found for this review question. 42 papers met the inclusion criteria. All were case series and many were retrospective. The study findings are varied with no strong evidence that any radiological parameter affects outcome. View here.
Evidence Statement
Level 3:
There is insufficient evidence in the literature to determine a meaningful association between any of the radiological parameters and patient rated outcome.
Recommendation
Grade of Recommendation: Grade D
Currently there is insufficient evidence to demonstrate a clear association between any measured radiological parameters and patient rated outcome. Further high quality research is required to answer this question.
The review has identified that the most commonly measured parameters were radial height, radial inclination, volar tilt, ulnar variance and intra articular step and gap. To investigate the influence of these radiological parameters on treatment decision making further, a Delphi study was organised. The Delphi method solicits the opinions of experts through a series of carefully designed questionnaires interspersed with information and opinion feedback in order to establish a convergence of opinion.
Delphi Study aims
- To identify which radiographic parameters are clinically important
- To quantify the threshold of displacement at which surgical intervention should take place for the commonly measured parameters
- To determine which patient factors influence the decision to intervene
Method
A Delphi study was completed with a panel of national and international experts who are experienced in the treatment of acute DRFs and their longer-term sequelae and/or have published clinical research investigating outcome after DRF.
Full ethical approval was obtained from the University of Leicester (Ethics Reference: 9559-nj94- healthsciences). The study protocol was registered with ClinicalTrials.gov (Identifier NCT03126474).
Delphi panel recruitment
The panel was composed of three groups of expert surgeons. Blue Book committee members were excluded. Many panel members fitted the criteria to belong in more than one of the following groups:
- Hand and wrist specialists – these surgeons would have considerable experience dealing with acute injuries and longer term problems after DRF. Participants were identified by sampling from UK BSSH members geographically.
- Trauma surgeons - those who deal acutely with patients with DRF and operate on them regularly. An email invitation was sent via the Orthopaedic Trauma Society (OTS) asking for volunteers to take part who fulfilled the above criteria.
- International researchers - surgeons who are also researchers and have published studies investigating outcome in patients with DRFs in the last 2 years so have a comprehensive understanding of the nature of the injury and likely outcome. A literature review of major orthopaedic and hand journals was carried out to identify potential participants.
Questions
Questions were based around six short case vignettes regarding a displaced extra-articular fracture in a 38, 58 and 75 year old patient, followed by a displaced intra-articular fracture in the same age groups. Those age groups were selected as it was considered that they would stimulate greater thought about decision making than if more extremes of age had been used.
Intervention was defined as any type of reduction and stabilisation, including manipulation and cast application.
Participants were asked to consider the functional outcome for each patient at three months after injury.
Question 1: Importance of parameters
Participants were asked to rank the parameters in order of importance on a visual analogue scale of 0 to 10 (0 = extremely unimportant, 10 = extremely important). Parameters were then ranked by median score and the results presented to the panel. Participants were asked if they agreed with the ranking. Consensus was defined as at least 70% agreement between participants.
Question 2: Thresholds for intervention
For each case vignette, panellists were asked at what measurement of displacement for each parameter they would intervene surgically. Agreement was then sought on the value at which intervention is required for each parameter by presenting the median value (from those scores independently offered in round one) alongside a scale of greater or lesser values. Where 70% agreed we accepted this as the point at which intervention should take place.
Question 3: Patient factors influencing decision making
Ten factors were presented to participants and they were asked to rate how important the factor is when deciding to intervene on a visual analogue scale of 0 to 10 (0 = extremely unimportant, 10 = extremely important). Factors were then ranked in order of importance by median score. A factor with a median score of three or less was accepted to be not important. A median score with an inter-quartile range of two or less was accepted as consensus for that score according to RAND criteria. Participants were asked if they agreed with the ranking. Consensus of the ranking was defined as at least 70% agreement between participants. Qualitative analysis was performed on the free text answers and comments. Stability of participants’ answers was analysed individually and between the three groups of panel members.
Results
Participant responses
56 surgeons were invited to take part. One declined and there was no response from nine after repeat reminders. 46 agreed to take part. 43 of those completed round one. All 43 who took part in round one then completed all rounds of the Delphi study.
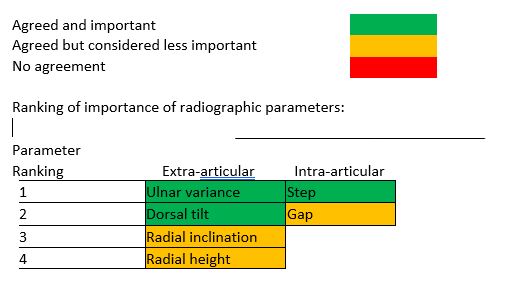
Question 1: Importance of parameters
Ulnar variance was consistently rated as the most important extra-articular parameter with dorsal tilt rated as the second most important for all age groups.
Intra-articular step (joint surfaces not aligned properly) was rated as the most important intra-articular parameter for all age groups. The panel agreed with these ranking orders for all parameters.
The following traffic light system is used to illustrate agreement and importance:
Question 2: Thresholds for intervention
Agreement denotes the percentage of the expert panel who would intervene at this radiographic threshold.
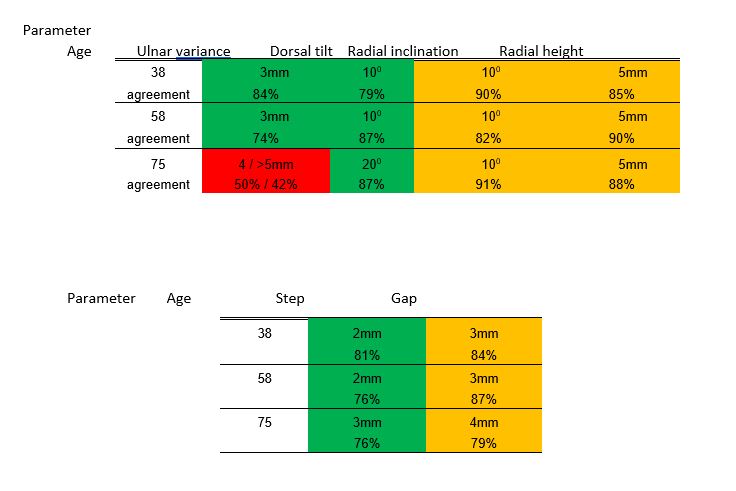
Consensus was obtained for all thresholds for intervention except ulnar variation in a 75 year old patient. For this case half of the panel would intervene at 4mm of positive ulnar variance whereas 42% would accept over 5mm of displacement.
Agreed thresholds were the same for all parameters for patients aged 38 and 58. There was no difference seen in thresholds between the three groups of participants
Question 3: Patient factors influencing decision making
Seven parameters were identified as important by the panel. Consensus was gained on the following rank order:
- Mental capacity
- Function
- Medical co-morbidities
- Age
- Compliance with rehabilitation
- Occupation
- Fragility
Consistency was seen between rounds indicating that panel members did not significantly change their choices throughout the rounds. There was no difference seen in preferences between the three groups of participants.
Qualitative review
Analysis of free text and comments revealed the following themes:
- Restoring function is the main aim of treatment.
- Establishing pre-injury function is consequently a significant factor in decision making.
- Assessment of function is multidimensional and will involve discussion with patient and carers, subjective judgement by clinician, and may include some standard assessment tools.
- Occupation is sometimes a factor.
- Comorbidities and mental capacity may illustrate functional level but are not influential in their own right.
- Independence is an important threshold in this assessment.
- Age may suggest broad treatment modalities but is less significant than function in individual cases.
- Assessment of compliance is sometimes a factor and mental capacity is a factor in this.
- Fragility may influence type of treatment but not the need for treatment.
Recommendation
Through this Delphi process our panel of experts agreed that ulnar variance and dorsal tilt are the most important extra-articular parameters and step is the most important intra-articular parameter. Consensus was gained on thresholds for intervention for all parameters for the three age groups except ulnar variance in a 75 year old patient. Seven patient factors were thought to be important regarding whether to intervene surgically and rank order of importance was agreed reflecting the preinjury functional state.
References:
ANAESTHESIA TECHNIQUES for MANIPULATION
|
Study
|
Intervention/ comparison
|
Patients
|
Outcomes
|
Comments
|
|
Funk (1997)
PRCT
|
GA vs haematoma +/- IV sedation
|
Adults (n=58)
|
Pain
Quality of Reduction (QOR)
|
QOR- No difference
Less pain post manipulation- haematoma block
No PROMS
|
INTRAVENOUS REGIONAL ANAESTHESIA (IVRA) VERSUS HAEMATOMA BLOCK – FIVE TRIALS.
|
Study
|
Intervention/ comparison
|
Patients
|
Outcomes
|
Comments
|
|
Abbaszadegan et al. (1990)
PRCT
|
IVRA vs haematoma block
|
Adults (n=99)
|
Quality of Reduction
ROM
Grip Strength
Pain
|
IVRA- Better & easier correction; Less post manipulation pain; Better grip strength
Similar ROM in both groups
|
|
Cobb et al. (1985)
PRCT
|
IVRA vs haematoma block
|
Adults (n=100)
|
Pain
Quality of Reduction (QOR)
|
Pain similar in both groups
Inadequate reduction rare and unrelated to method of anaesthesia
|
|
Kendall et al. (1997)
PRCT
Add level of evidence
|
IVRA vs haematoma block
|
Adults (n=150)
|
Pain
Quality of Reduction (QOR)
|
IVRA- Better & easier correction; Less post manipulation pain
|
|
Walther-Larsen et al. (1988)
PRCT
|
IVRA vs haematoma block
|
Adults (n=48)
|
Pain
QOR
ROM
Grip Strength
|
IVRA- Better & easier correction
No functional difference
|
|
Wardrope et al. (1985)
PRCT
|
IVRA vs haematoma block
|
Adults (n=81)
|
Pain
Quality of Reduction (QOR)
|
IVRA- Better & easier correction
|
Back
|
Study
|
Intervention/ comparison
|
Patients
|
Outcomes
|
Comments
|
|
Kelly et al. (2009)
PRCT
|
Closed reduction vs no reduction
|
Adults (n=60)
|
Gartland & Werley
Grip Strength
Radiological position
Cosmesis
CRPS
|
Patients aged ≥65 years with moderately displaced fractures
There was no detectable difference between the groups in any of the outcome measures
|
|
Handoll et al. (2002)
Systematic Review
|
Closed reduction vs no reduction
|
Adults (n=60)
|
Gartland & Werley
Grip Strength
Radiological position
Cosmesis
CRPS
|
Manipulation was unnecessary in selected elderly patients with only moderately displaced fractures.
There is no conclusive evidence of difference in outcome between
reduction or no reduction of displaced fractures
Findings based on the study by Kelly et al only
|
|
Study
|
Intervention/ comparison
|
Patients
|
Outcomes
|
Comments
|
|
Wik et al. (2008)
PRCT
|
Complete plaster cast vs dorsal plaster splint
|
Adults (n=72 all females)
|
Pain
Radiological parameters for maintenance of reduction
|
Pain:
Day 1 more cast group; Day 10- no difference
Split/Release for Tightness: equal number
Reduction at Day 10:
slab-better for dorsal angulation cast-better for radial length
|
VITAMIN C FOR PREVENTION OF COMPLEX REGIONAL PAIN SYNDROME (CRPS)
|
Study
|
Intervention/ comparison
|
Patients
|
Outcomes
|
Comments
|
|
Evaniew et al. (2015)
Meta-analysis
|
Vitamin C v placebo
|
Adults (n=890)
|
CRPS incidence
|
There is no evidence for vitamin C to prevent CRPS in patients with distal radius fractures
Overall quality of evidence is low
|
|
Meena et al. (2015)
Meta-analysis
|
Vitamin C
|
Adults (n=810)
|
CRPS incidence
|
Significant reduction in the prevalence of CRPS with the use of vitamin C
|
|
Shibuya et al. (2013)
Meta-analysis
|
Vitamin C(500mg+)
|
Adults (n=616)
|
CRPS incidence
Complications
|
Meta analysis was carried out to investigate effectiveness of Vitamin C in foot and ankle surgery and trauma
Three out of the four studies included looked at distal radius fracture patients only
Vitamin C may be beneficial in foot and ankle surgery or injury to avoid CRPS
|
- Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthop. 2008 Jun;79(3):376-85.
- Altissimi M, Antenucci R, Fiacca C, Mancini GB. Long-term results of conservative treatment of fractures of the distal radius. Clin Orthop Relat Res. 1986 May;(206):202-10.
- Anzarut A, Johnson JA, Rowe BH, Lambert RGW, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004 Nov;29(6):1121-7.
- Aro HT, Koivunen T. Minor axial shortening of the radius affects outcome of Colles' fracture treatment. J Hand Surg Am. 1991 May;16(3):392-398.
- Barton T, Chambers C, Bannister G. A comparison between subjective outcome score and moderate radial shortening following a fractured distal radius in patients of mean age 69 years. J Hand Surg Eur. 2007 Apr;32(2):165-9.
- Batra S, Gupta A. The effect of fracture-related factors on the functional outcome at 1 year in distal radius fractures. Injury. 2002 Jul;33(6):499-502.
- Bentohami A, Bijlsma TS, Goslings JC, de Reuver P, Kaufmann L, Schep NW. Radiological criteria for acceptable reduction of extra-articular distal radial fractures are not predictive for patient-reported functional outcome. J Hand Surg Eur Vol. 2013 Jun;38(5):524-9.
- Beumer A, Adlercreutz C, Lindau T. Early prognostic factors in distal radius fractures in a younger than osteoporotic age group: a multivariate analysis of trauma radiographs. BMC Musculoskelet Disord. 2013 May 22;14:170.
- Braziulis K, Rimdeika R, Kregzdyte R, Tarasevicius S. Associations between the fracture type and functional outcomes after distal radial fractures treated with a volar locking plate. Medicina (Kaunas). 2013;49(9):399-402.
- Brogren E, Hofer M, Petranek M, Wagner P, Dahlin B, Atroshi I. Relationship between distal radius fracture malunion and arm-related disability: A prospective population based cohort study with 1-year follow-up. BMC Musculoskelet Disord. 2011 Jan 13; 12:9.
- Choi WS, Lee HJ, Kim DY, Lee CH, Lee BG, Kim JH, Lee KH. Does osteoporosis have a negative effect on the functional outcome of an osteoporotic distal radial fracture treated with a volar locking plate? Bone Joint J. 2015 Feb;97-B(2):229-234.
- Chung KC, Kotsis SV, Kim HM. Predictors of Functional Outcomes After Surgical Treatment of Distal Radius Fractures. J Hand Surg Am. 2007 Jan;32(1):76-83.
- Dario P, Matteo G, Carolina C, Marco G, Cristina D, Daniele F, Andrea F. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. 2014 Dec; 45 Suppl 6:S21-6.
- Dixon S, Allen P, Bannister G. Which Colles' fractures should be manipulated? Injury. 2005 Jan;36(1):81-3.
- Fernandez JJ, Gruen GS, Herndon JH. Outcome of distal radius fractures using the short form 36 health survey. Clin Orthop Relat Res. 1997 Aug;(341):36-41.
- Finsen V, Rod O, Rød K, Rajabi B, Alm-Paulsen PS, Russwurm H. The relationship between displacement and clinical outcome after distal radius (Colles') fracture. Journal Hand Surg Eur Vol. 2013 Feb;38(2):116-26.
- Foldhazy Z, Tornkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L. Long-term outcome of nonsurgically treated distal radius fractures. J Hand Surg Am. 2007 Nov;32(9):1374-1384.
- Forward DP, Davis TRC, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008 May;(5):629-37.
- Fujii K, Henmi T, Kanematsu Y, Mishiro T, Sakai T, Terai T. Fractures of the distal end of radius in elderly patients: a comparative study of anatomical and functional results. J Orthop Surg (Hong Kong). 2002 Jun;10(1):9-15.
- Gavaskar AS, Muthukumar S, Chowdary N. Fragment-specific fixation for complex intra-articular fractures of the distal radius: results of a prospective single-centre trial. J Hand Surg Eur Vol. 2012 Oct;37(8);765-71.
- Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radius fracture in young adults. J Hand Surg Br. 2000 Dec;25(6):535-43.
- Grewal R, Macdermid J, Pope J, Chesworth B. Baseline predictors of pain and disability one year following extra-articular distal radius fractures. Hand (N Y). 2007 Sep;2(3):104–11.
- Hollevoet N, Verdonk R. The functional importance of malunion in distal radius fractures. Acta Orthop Belg. 2003 June;69(3):239-45.
- Jaremko JL, Lambert RG, Rowe BH, Johnson JA, Majumdar SR. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment Clin Radiol. 2007 Jan;62(1):65-72.
- Jenkins NH, Mintowt-Czyz WJ. Mal-union and dysfunction in Colles' fracture J Hand Surg Br. 1988 Aug;13(3):291-3.
- Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005 Dec;36(12):1435-9.
- Kodama N, Takemura Y, Ueba H, Imai S, Matsusue Y. Acceptable parameters for alignment of distal radius fracture with conservative treatment in elderly patients J Orthop Sci. 2014 Mar;19(2):292-7.
- Kopylov P, Johnell O, Redlund-Johnell I, Bengner U. Fractures of the distal end of the radius in young adults: a 30-year follow-up J Hand Surg Br. 1993 Feb;18(1):45-9.
- Kumar S, Penematsa S, Sadri M, Deshmukh SC. Can radiological results be surrogate markers of functional outcome in distal radial extra-articular fractures? Int Orthop. 2008 Aug;32(4):505-9.
- Leung F, Ozkan M, Chow SP. Conservative treatment of intra-articular fractures of the distal radius--factors affecting functional outcome. Hand Surg. 2000 Dec;5(2):145-53.
- MacDermid JC, Donner A, Richards RS, Roth JH. Patient versus injury factors as predictors of pain and disability six months after a distal radius fracture. J Clin Epidemiol. 2002 Sep;55(9):849-54.
- Porter M, Stockley I. Fractures of the distal radius. Intermediate and end results in relation to radiologic parameters. Clin Orthop Relat Res. 1987 Jul;(220):241-52.
- Sammer DM, Shah HM, Shauver MJ, Chung KC. The effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am. 2009 Nov;34(9):1595-602.
- Smilovic J, Bilic R. Conservative treatment of extra-articular Colles' type fractures of the distal radius: prospective study. Croat Med J. 2003 Dec;44(6):740-5.
- Solgaard S. Function after distal radius fracture. Acta Orthop Scand. 1988 Feb;59(1):39-42.
- Stewart HD, Innes AR, Burke FD. Factors affecting the outcome of Colles' fracture: an anatomical and functional study. Injury. 1985 Mar;16(5):289-95.
- Synn AJ, Makhni EC, Makhni MC, Rozental TD, Day CS. Distal radius fractures in older patients: Is anatomic reduction necessary? Clin Orthop Relat Res. 2009 Jun;467(6):1612-20.
- Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994 Mar;19(2):325-40.
- Tsukazaki T, Takagi K, Iwasaki K. Poor correlation between functional results and radiographic findings in Colles' fracture. J Hand Surg Br. 1993 Oct;18(5):588-91.
- Villar RN, Marsh D, Rushton N, Greatorex RA. Three years after Colles' fracture. A prospective review. J Bone Joint Surg Br. 1987 Aug;69(4):635-8.
- Warwick D, Field J, Prothero D, Gibson A, Bannister GC. Function ten years after Colles' fracture. Clin Orthop Relat Res. 1993 Oct;(295):270-4.
- Wilcke MK, Abbaszadegan H, Adolphson PY. Patient-perceived outcome after displaced distal radius fractures: a comparison between radiological parameters,objective physical variables, and the DASH score. J Hand Ther. 2007 Oct-Dec;20(4):290-8; quiz 299,